Bone marrow is like the offensive line of the immune system — it’s an essential part of the team but doesn’t always gets the recognition. By pumping out hundreds of billions of blood cells every day, bone marrow helps us fend off disease and is essential to a healthy human body.
To better understand how marrow fortifies us against disease — and to potentially help develop better therapies for diseases like leukemia — researchers have sought to develop artificial bone marrow that functions like the real thing. The problem is, living blood cells reside and multiply in a special environment, called the hematopoietic niche, which scientists have so far failed to replicate.
But now, researchers from the University of Basel and ETH Zurich have engineered an artificial bone marrow that mimics the natural kinds, offering a key to better understand how blood forms and how blood diseases can be treated.
“This 3D engineered tissue is established and maintained in a bioreactor system,” Ivan Martin, a professor of biomedicine at the University of Basel who worked on the project, told Digital Trends. “It partially recapitulates the structure, composition, and organization of the native bone marrow microenvironment … but also its main function, which is the replication and differentiation in more mature cells.”
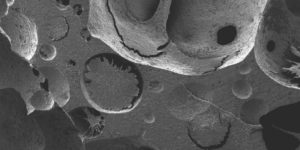
Martin and his colleagues used a ceramic bonelike scaffold, which they combined with living cells in a bioreactor, mixing the synthetic and organic components together.
Within that artificial system, cells are able to multiply over the course of several days — not as long as natural bone marrow, but degrees better than previous synthetic models. Rather than immediate medical applications, the researchers hope their technique leads to more sophisticated, tailor-made marrow models, which can assist in drug screening.
“More than a direct medical demand, the fields of hematology and tissue engineering lacked a model close enough to sustain reasonable comparison with the in vivo human bone marrow microenvironment,” Matin said. “Indeed, research has limited possibilities to access information from human specimens and the human hematopoietic niche has remained rather inaccessible to experimental manipulation and optical observation.”
Moving forward, Martin and his team hope to use this system to study blood disorders, particularly the conditions within which these conditions first arise.
A paper detailing their research was published this week in the journal Proceeding of the National Academy of Sciences.


